Stress, Hormones & Belly Fat The Female Connection
Ever wondered why belly fat seems to “suddenly show up” and refuses to leave even when you’re eating right and moving your body?
For many women, the answer isn’t just calories… it’s hormones and stress.
How Stress Changes a Woman’s Body
When you’re stressed whether from work, family, relationships, finances, or even silent emotional pressure your body produces a hormone called cortisol.
In small doses, cortisol helps you handle challenges. But when stress becomes constant, cortisol stays high. And here’s the tricky part:
> High cortisol tells your body to store fat especially around your belly.
Hormones That Play a Big Role
Women’s bodies are constantly navigating hormonal shifts from puberty to pregnancy to perimenopause and menopause. The key players include:
Cortisol ;stress hormone → increases belly fat
Estrogen; when it drops, the body stores more fat in the abdomen
Insulin; affected by sugar intake and stress, leads to fat storage
Leptin; hunger hormone, disrupted by poor sleep and stress
So no, you’re not “lazy.”
Your body may simply be responding to stress and hormonal changes.
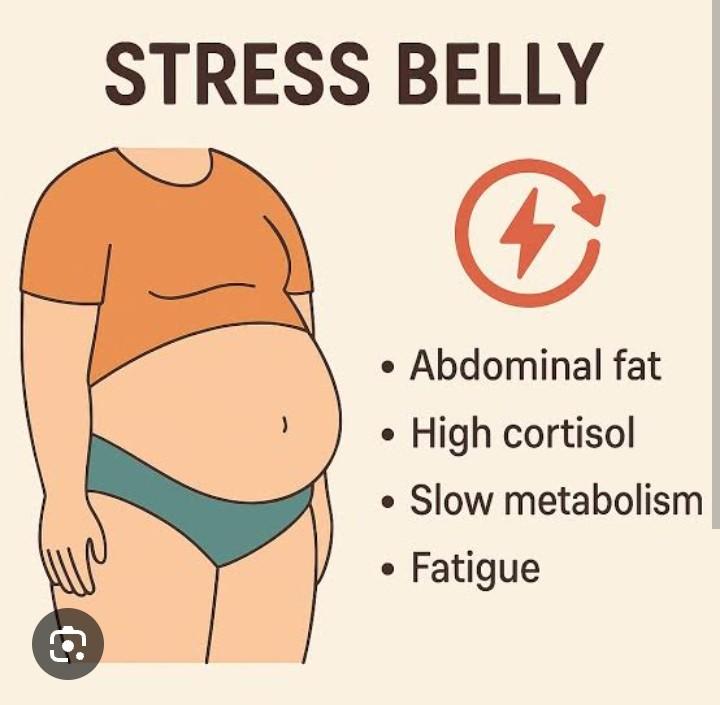
Common Signs Stress & Hormones Are Affecting Your Belly
You may notice:
1. Weight gain mainly around the stomach
2. Cravings for sugary or salty snacks
3. Tiredness even after sleeping
4. Mood changes or anxiety
5. Bloating and sluggish digestion
These are real signals not excuses.
How to Fight Stress-Related Belly Fat
You don’t need extreme dieting. Focus on balance:
Prioritize 7-8 hours of sleep
Eat protein, fiber, and healthy fats (keeps hormones steady)
Reduce caffeine & sugary snacks
Practice breathing exercises or journaling
Move your body daily, walking counts
Avoid starvation diets ,they increase cortisol
Bottom Line
Belly fat in women is not just about food or exercise, it’s deeply connected to stress and hormones.
Understanding this helps you approach your body with patience and respect, not frustration.
Your body is not fighting you , it’s protecting you.
Support it gently…and it will respond
Ever wondered why belly fat seems to “suddenly show up” and refuses to leave even when you’re eating right and moving your body?
For many women, the answer isn’t just calories… it’s hormones and stress.
How Stress Changes a Woman’s Body
When you’re stressed whether from work, family, relationships, finances, or even silent emotional pressure your body produces a hormone called cortisol.
In small doses, cortisol helps you handle challenges. But when stress becomes constant, cortisol stays high. And here’s the tricky part:
> High cortisol tells your body to store fat especially around your belly.
Hormones That Play a Big Role
Women’s bodies are constantly navigating hormonal shifts from puberty to pregnancy to perimenopause and menopause. The key players include:
Cortisol ;stress hormone → increases belly fat
Estrogen; when it drops, the body stores more fat in the abdomen
Insulin; affected by sugar intake and stress, leads to fat storage
Leptin; hunger hormone, disrupted by poor sleep and stress
So no, you’re not “lazy.”
Your body may simply be responding to stress and hormonal changes.
Common Signs Stress & Hormones Are Affecting Your Belly
You may notice:
1. Weight gain mainly around the stomach
2. Cravings for sugary or salty snacks
3. Tiredness even after sleeping
4. Mood changes or anxiety
5. Bloating and sluggish digestion
These are real signals not excuses.
How to Fight Stress-Related Belly Fat
You don’t need extreme dieting. Focus on balance:
Prioritize 7-8 hours of sleep
Eat protein, fiber, and healthy fats (keeps hormones steady)
Reduce caffeine & sugary snacks
Practice breathing exercises or journaling
Move your body daily, walking counts
Avoid starvation diets ,they increase cortisol
Bottom Line
Belly fat in women is not just about food or exercise, it’s deeply connected to stress and hormones.
Understanding this helps you approach your body with patience and respect, not frustration.
Your body is not fighting you , it’s protecting you.
Support it gently…and it will respond
Stress, Hormones & Belly Fat The Female Connection
Ever wondered why belly fat seems to “suddenly show up” and refuses to leave even when you’re eating right and moving your body?
For many women, the answer isn’t just calories… it’s hormones and stress.
How Stress Changes a Woman’s Body
When you’re stressed whether from work, family, relationships, finances, or even silent emotional pressure your body produces a hormone called cortisol.
In small doses, cortisol helps you handle challenges. But when stress becomes constant, cortisol stays high. And here’s the tricky part:
> High cortisol tells your body to store fat especially around your belly.
Hormones That Play a Big Role
Women’s bodies are constantly navigating hormonal shifts from puberty to pregnancy to perimenopause and menopause. The key players include:
Cortisol ;stress hormone → increases belly fat
Estrogen; when it drops, the body stores more fat in the abdomen
Insulin; affected by sugar intake and stress, leads to fat storage
Leptin; hunger hormone, disrupted by poor sleep and stress
So no, you’re not “lazy.”
Your body may simply be responding to stress and hormonal changes.
Common Signs Stress & Hormones Are Affecting Your Belly
You may notice:
1. Weight gain mainly around the stomach
2. Cravings for sugary or salty snacks
3. Tiredness even after sleeping
4. Mood changes or anxiety
5. Bloating and sluggish digestion
These are real signals not excuses.
How to Fight Stress-Related Belly Fat
You don’t need extreme dieting. Focus on balance:
✅ Prioritize 7-8 hours of sleep
✅ Eat protein, fiber, and healthy fats (keeps hormones steady)
✅ Reduce caffeine & sugary snacks
✅ Practice breathing exercises or journaling
✅ Move your body daily, walking counts
✅ Avoid starvation diets ,they increase cortisol
Bottom Line
Belly fat in women is not just about food or exercise, it’s deeply connected to stress and hormones.
Understanding this helps you approach your body with patience and respect, not frustration.
Your body is not fighting you , it’s protecting you.
Support it gently…and it will respond
0 Comments
0 Shares
115 Views