Passionate about health and fitness, I share simple, practical tips to help you live a healthier, happier life.
From daily habits to fitness motivation, I’m here to make wellness easy and enjoyable. Let’s take small steps toward a better you!
From daily habits to fitness motivation, I’m here to make wellness easy and enjoyable. Let’s take small steps toward a better you!
-
42 Posts
-
41 Photos
-
0 Videos
-
Lives in Enugu
-
From Nkanu East
-
Studied Medical Rehabilitation at UnecClass of 300 level
-
Female
-
Single
-
Followed by 2 people
Recent Updates
-
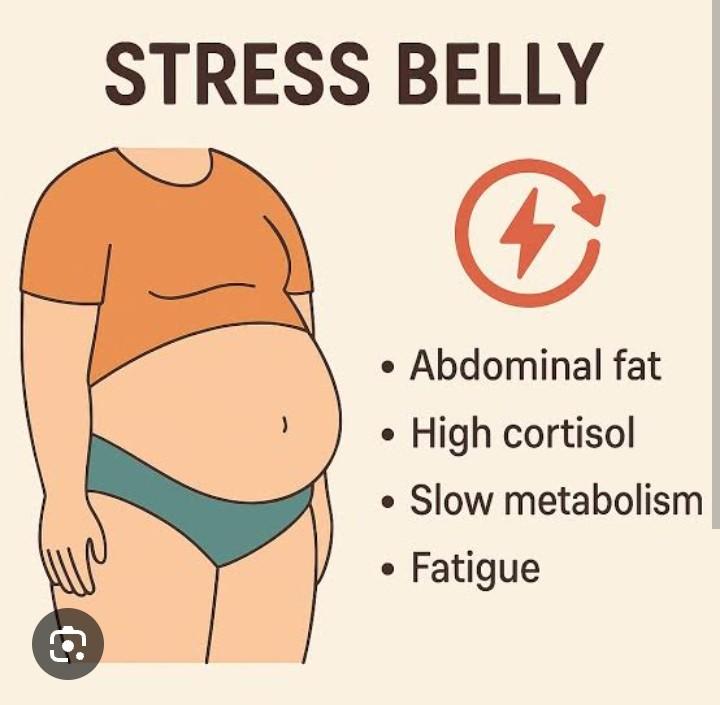
Stress, Hormones & Belly Fat The Female Connection
Ever wondered why belly fat seems to “suddenly show up” and refuses to leave even when you’re eating right and moving your body?
For many women, the answer isn’t just calories… it’s hormones and stress.
How Stress Changes a Woman’s Body
When you’re stressed whether from work, family, relationships, finances, or even silent emotional pressure your body produces a hormone called cortisol.
In small doses, cortisol helps you handle challenges. But when stress becomes constant, cortisol stays high. And here’s the tricky part:
> High cortisol tells your body to store fat especially around your belly.
Hormones That Play a Big Role
Women’s bodies are constantly navigating hormonal shifts from puberty to pregnancy to perimenopause and menopause. The key players include:
Cortisol ;stress hormone → increases belly fat
Estrogen; when it drops, the body stores more fat in the abdomen
Insulin; affected by sugar intake and stress, leads to fat storage
Leptin; hunger hormone, disrupted by poor sleep and stress
So no, you’re not “lazy.”
Your body may simply be responding to stress and hormonal changes.
Common Signs Stress & Hormones Are Affecting Your Belly
You may notice:
1. Weight gain mainly around the stomach
2. Cravings for sugary or salty snacks
3. Tiredness even after sleeping
4. Mood changes or anxiety
5. Bloating and sluggish digestion
These are real signals not excuses.
How to Fight Stress-Related Belly Fat
You don’t need extreme dieting. Focus on balance:
Prioritize 7-8 hours of sleep
Eat protein, fiber, and healthy fats (keeps hormones steady)
Reduce caffeine & sugary snacks
Practice breathing exercises or journaling
Move your body daily, walking counts
Avoid starvation diets ,they increase cortisol
Bottom Line
Belly fat in women is not just about food or exercise, it’s deeply connected to stress and hormones.
Understanding this helps you approach your body with patience and respect, not frustration.
Your body is not fighting you , it’s protecting you.
Support it gently…and it will respondStress, Hormones & Belly Fat The Female Connection Ever wondered why belly fat seems to “suddenly show up” and refuses to leave even when you’re eating right and moving your body? For many women, the answer isn’t just calories… it’s hormones and stress. How Stress Changes a Woman’s Body When you’re stressed whether from work, family, relationships, finances, or even silent emotional pressure your body produces a hormone called cortisol. In small doses, cortisol helps you handle challenges. But when stress becomes constant, cortisol stays high. And here’s the tricky part: > High cortisol tells your body to store fat especially around your belly. Hormones That Play a Big Role Women’s bodies are constantly navigating hormonal shifts from puberty to pregnancy to perimenopause and menopause. The key players include: Cortisol ;stress hormone → increases belly fat Estrogen; when it drops, the body stores more fat in the abdomen Insulin; affected by sugar intake and stress, leads to fat storage Leptin; hunger hormone, disrupted by poor sleep and stress So no, you’re not “lazy.” Your body may simply be responding to stress and hormonal changes. Common Signs Stress & Hormones Are Affecting Your Belly You may notice: 1. Weight gain mainly around the stomach 2. Cravings for sugary or salty snacks 3. Tiredness even after sleeping 4. Mood changes or anxiety 5. Bloating and sluggish digestion These are real signals not excuses. How to Fight Stress-Related Belly Fat You don’t need extreme dieting. Focus on balance: ✅ Prioritize 7-8 hours of sleep ✅ Eat protein, fiber, and healthy fats (keeps hormones steady) ✅ Reduce caffeine & sugary snacks ✅ Practice breathing exercises or journaling ✅ Move your body daily, walking counts ✅ Avoid starvation diets ,they increase cortisol Bottom Line Belly fat in women is not just about food or exercise, it’s deeply connected to stress and hormones. Understanding this helps you approach your body with patience and respect, not frustration. Your body is not fighting you , it’s protecting you. Support it gently…and it will respond0 Comments 0 Shares 171 ViewsPlease log in to like, share and comment! -
“Stroke Doesn’t Knock , It Crashes In: What You Need to Know Before It’s Too Late”
Stroke is one of those health issues many people think only happens to “older people.”
Until suddenly, it’s not just a headline it’s a family member, a friend, someone at church, a colleague… or even a young person on social media.
The truth?
Stroke is no longer an “old age problem.”
Stress-filled lifestyles, high blood pressure, smoking, poor diet, and even untreated infections are bringing it closer and faster.
A stroke happens when the blood flow to the brain is blocked or a blood vessel bursts.
And because the brain controls everything, one moment can change everything movement, speech, memory, even personality.
So How Do Strokes Show Up?
A stroke doesn’t always come with drama. Sometimes it whispers before it screams.
Watch out for sudden:
Weakness or numbness on one side of the body
Drooping face or slurred speech
Trouble understanding others
Loss of balance or confusion
Severe headache out of nowhere
Use the FAST rule:
F – Face: Is one side dropping?
A – Arms: Can they raise both?
S – Speech: Slurred or strange?
T – Time: Rush to the hospital immediately every minute matters.
Why Younger People Are at Risk Now
Let’s be honest modern habits aren’t helping us:
Constant stress & overthinking
High blood pressure (often undiagnosed)
Too much salt and processed food
Smoking & alcohol
Sitting more than we move
Ignoring headaches and dizziness
Poor sleep and dehydration
A lot of us feel tired but push through, saying “I’ll be fine.”
Your body hears you but one day, it might respond differently.
How to Protect Yourself
No extreme diet or expensive detox needed. Just intentional living:
Check your blood pressure regularly
Eat less salty & oily foods
Stay hydrated
Move your body even a 20 minutes walk helps
Reduce alcohol & avoid smoking
Take stress breaks your brain needs rest too
Treat headaches and dizziness seriously
Visit the hospital if something feels “off”
Small habits save lives literally.
Final Thought
Stroke doesn’t send a warning letter.
It doesn’t wait for you to “finish that task first.”
Your health is not an inconvenience ;t’s your life.
Listen to your body before it forces you to stop.“Stroke Doesn’t Knock , It Crashes In: What You Need to Know Before It’s Too Late” Stroke is one of those health issues many people think only happens to “older people.” Until suddenly, it’s not just a headline it’s a family member, a friend, someone at church, a colleague… or even a young person on social media. The truth? Stroke is no longer an “old age problem.” Stress-filled lifestyles, high blood pressure, smoking, poor diet, and even untreated infections are bringing it closer and faster. A stroke happens when the blood flow to the brain is blocked or a blood vessel bursts. And because the brain controls everything, one moment can change everything movement, speech, memory, even personality. So How Do Strokes Show Up? A stroke doesn’t always come with drama. Sometimes it whispers before it screams. Watch out for sudden: Weakness or numbness on one side of the body Drooping face or slurred speech Trouble understanding others Loss of balance or confusion Severe headache out of nowhere Use the FAST rule: F – Face: Is one side dropping? A – Arms: Can they raise both? S – Speech: Slurred or strange? T – Time: Rush to the hospital immediately every minute matters. Why Younger People Are at Risk Now Let’s be honest modern habits aren’t helping us: Constant stress & overthinking High blood pressure (often undiagnosed) Too much salt and processed food Smoking & alcohol Sitting more than we move Ignoring headaches and dizziness Poor sleep and dehydration A lot of us feel tired but push through, saying “I’ll be fine.” Your body hears you but one day, it might respond differently. How to Protect Yourself No extreme diet or expensive detox needed. Just intentional living: Check your blood pressure regularly Eat less salty & oily foods Stay hydrated Move your body even a 20 minutes walk helps Reduce alcohol & avoid smoking Take stress breaks your brain needs rest too Treat headaches and dizziness seriously Visit the hospital if something feels “off” Small habits save lives literally. Final Thought Stroke doesn’t send a warning letter. It doesn’t wait for you to “finish that task first.” Your health is not an inconvenience ;t’s your life. Listen to your body before it forces you to stop.0 Comments 0 Shares 289 Views -
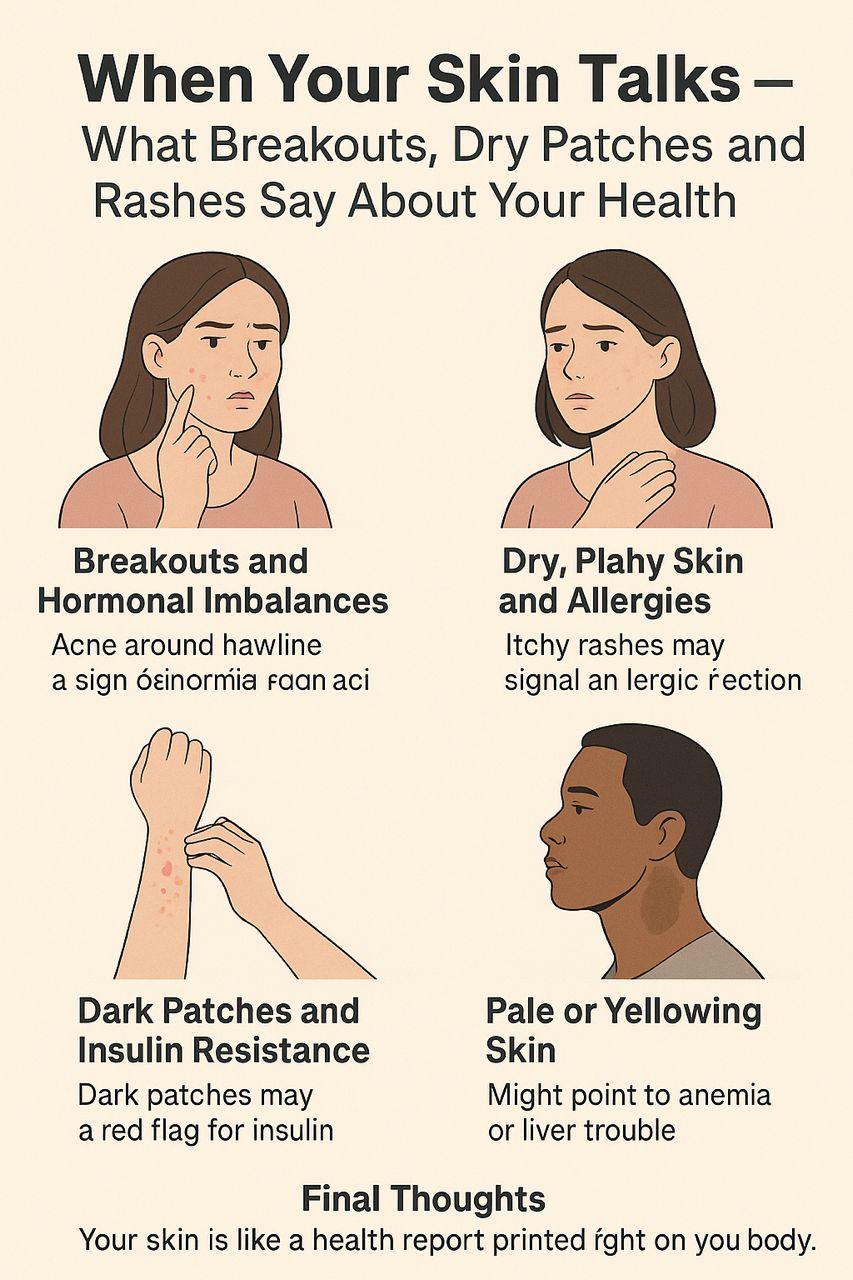
Title: When Your Skin Talks — What Breakouts, Dry Patches, and Rashes Say About Your Health
Your skin does more than just shield your body it speaks. That stubborn breakout on your chin or the unexplained dryness on your elbows might be more than a skincare issue. It might be your body trying to tell you something.
Breakouts and Hormonal Imbalances
Acne that keeps showing up around your jawline and chin area can be a sign of hormonal fluctuations. This is especially common during menstruation, pregnancy, or in conditions like polycystic ovarian syndrome (PCOS). If topical treatments don’t help, it might be time to look inward literally.
Dry, Flaky Skin and Dehydration
When your skin feels like sandpaper despite regular moisturizing, the issue could be inside. Dehydration and underactive thyroid (hypothyroidism) are common causes. Drinking more water, improving your diet, and checking your thyroid levels can make a difference.
Itchy Rashes and Allergies
Sudden rashes, especially when itchy or inflamed, can signal an allergic reaction to something you ate, touched, or inhaled. Eczema and psoriasis are also signs of immune system overactivity and can flare up due to stress or poor gut health.
Dark Patches and Insulin Resistance
Patches of darkened skin, especially around the neck, armpits, or groin (called acanthosis nigricans), can be a red flag for insulin resistance. This condition is a warning sign for prediabetes or type 2 diabetes. It's best not to ignore it.
Pale or Yellowing Skin
Skin that looks unusually pale might point to anemia, while yellowish tones could suggest liver trouble. Both are worth checking out with a healthcare provider, especially if they come with fatigue or other symptoms.
Final Thoughts
Your skin is like a health report printed right on your body. When something changes, don’t just reach for a cream listen carefully. It might be telling you that something deeper needs attention.
Healthy skin starts with a healthy you.Title: When Your Skin Talks — What Breakouts, Dry Patches, and Rashes Say About Your Health Your skin does more than just shield your body it speaks. That stubborn breakout on your chin or the unexplained dryness on your elbows might be more than a skincare issue. It might be your body trying to tell you something. Breakouts and Hormonal Imbalances Acne that keeps showing up around your jawline and chin area can be a sign of hormonal fluctuations. This is especially common during menstruation, pregnancy, or in conditions like polycystic ovarian syndrome (PCOS). If topical treatments don’t help, it might be time to look inward literally. Dry, Flaky Skin and Dehydration When your skin feels like sandpaper despite regular moisturizing, the issue could be inside. Dehydration and underactive thyroid (hypothyroidism) are common causes. Drinking more water, improving your diet, and checking your thyroid levels can make a difference. Itchy Rashes and Allergies Sudden rashes, especially when itchy or inflamed, can signal an allergic reaction to something you ate, touched, or inhaled. Eczema and psoriasis are also signs of immune system overactivity and can flare up due to stress or poor gut health. Dark Patches and Insulin Resistance Patches of darkened skin, especially around the neck, armpits, or groin (called acanthosis nigricans), can be a red flag for insulin resistance. This condition is a warning sign for prediabetes or type 2 diabetes. It's best not to ignore it. Pale or Yellowing Skin Skin that looks unusually pale might point to anemia, while yellowish tones could suggest liver trouble. Both are worth checking out with a healthcare provider, especially if they come with fatigue or other symptoms. Final Thoughts Your skin is like a health report printed right on your body. When something changes, don’t just reach for a cream listen carefully. It might be telling you that something deeper needs attention. Healthy skin starts with a healthy you.0 Comments 0 Shares 868 Views -
“When Sadness Lingers: Could It Be More Than Just a Bad Day?”
Everyone feels sad from time to time. Maybe it’s a stressful week, a missed opportunity, or just one of those days when nothing seems right. That’s normal. But what happens when the sadness doesn’t go away? When you wake up feeling empty, unmotivated, or exhausted day after day?
Let’s talk about what it means when sadness lingers, and how to know when it’s more than just a bad day.
It’s Not Just in Your Head
Many people downplay how they feel. “I’m just being dramatic,” or “I’ll be fine tomorrow.” But persistent sadness can affect more than just your mood it can impact your physical health too. You may notice:
Low energy, even after resting
Changes in appetite or sleep (too much or too little)
Difficulty focusing or making decisions
Aches and pains with no clear cause
Feeling numb, irritable, or hopeless
These are real symptoms. And they’re not your fault,
When Sadness Becomes Depression
Depression doesn’t always look the way we expect. Some people cry a lot, while others feel flat and disconnected. Some keep functioning going to work, caring for family but feel like they’re just surviving, not living.
If you’ve been feeling this way for more than two weeks, it could be a sign of clinical depression. And that’s a health condition, not a weakness. Like any illness, it deserves attention and care.
What Causes It?
Depression doesn’t always have a clear cause. It can be triggered by life events like grief, trauma, or burnout but sometimes, it happens without warning. Genetics, brain chemistry, and even hormonal changes (like after childbirth or during menstruation) can play a role.
The important thing to remember is: You don’t need a reason to feel the way you feel.
What Can You Do?
If this sounds familiar, you’re not alone and you’re not stuck.
Talk to someone: A friend, loved one, counselor, or doctor. Talking helps.
Seek professional help: Therapists and mental health professionals can offer support and treatment.
Don’t ignore your body: Eat well, move your body, and get sunlight even small steps matter.
Give yourself grace: Healing takes time, and it’s okay to ask for help.
Final Thoughts
We all have hard days, but if your “off days” are turning into off weeks or months, it’s worth listening to what your body and mind are telling you. There’s no shame in struggling and there’s always a path to feeling better.
Because sometimes, it’s not just a bad day. And that’s okay.“When Sadness Lingers: Could It Be More Than Just a Bad Day?” Everyone feels sad from time to time. Maybe it’s a stressful week, a missed opportunity, or just one of those days when nothing seems right. That’s normal. But what happens when the sadness doesn’t go away? When you wake up feeling empty, unmotivated, or exhausted day after day? Let’s talk about what it means when sadness lingers, and how to know when it’s more than just a bad day. It’s Not Just in Your Head Many people downplay how they feel. “I’m just being dramatic,” or “I’ll be fine tomorrow.” But persistent sadness can affect more than just your mood it can impact your physical health too. You may notice: Low energy, even after resting Changes in appetite or sleep (too much or too little) Difficulty focusing or making decisions Aches and pains with no clear cause Feeling numb, irritable, or hopeless These are real symptoms. And they’re not your fault, When Sadness Becomes Depression Depression doesn’t always look the way we expect. Some people cry a lot, while others feel flat and disconnected. Some keep functioning going to work, caring for family but feel like they’re just surviving, not living. If you’ve been feeling this way for more than two weeks, it could be a sign of clinical depression. And that’s a health condition, not a weakness. Like any illness, it deserves attention and care. What Causes It? Depression doesn’t always have a clear cause. It can be triggered by life events like grief, trauma, or burnout but sometimes, it happens without warning. Genetics, brain chemistry, and even hormonal changes (like after childbirth or during menstruation) can play a role. The important thing to remember is: You don’t need a reason to feel the way you feel. What Can You Do? If this sounds familiar, you’re not alone and you’re not stuck. Talk to someone: A friend, loved one, counselor, or doctor. Talking helps. Seek professional help: Therapists and mental health professionals can offer support and treatment. Don’t ignore your body: Eat well, move your body, and get sunlight even small steps matter. Give yourself grace: Healing takes time, and it’s okay to ask for help. Final Thoughts We all have hard days, but if your “off days” are turning into off weeks or months, it’s worth listening to what your body and mind are telling you. There’s no shame in struggling and there’s always a path to feeling better. Because sometimes, it’s not just a bad day. And that’s okay.0 Comments 0 Shares 835 Views -
Tired But Can’t Sleep? The Hidden Link Between Anxiety and Insomnia
Ever crawl into bed, physically exhausted, but your mind just won’t shut up? You toss. You turn. You check the clock. Again. And despite needing rest more than ever, your body refuses to power down. Sound familiar?
You’re not alone and you’re not just “thinking too much.” This frustrating cycle of being tired but sleepless is often rooted in anxiety, and the connection runs deeper than most people realize.
The Silent Tug-of-War Between Your Mind and Body
When you’re anxious whether it's from everyday stress or a deeper mental health issue your brain kicks into high alert. Your heart rate might stay elevated. Your thoughts start racing. Your body stays in “fight or flight” mode, even when it’s bedtime. And no matter how tired you feel, your brain acts like it’s preparing for battle.
It’s like hitting the brakes and the gas pedal at the same time.
Everyday Habits That Make It Worse
Without even knowing it, some of our daily routines quietly feed this cycle. For example:
Endless scrolling before bed overstimulates the brain and floods your system with blue light, which blocks melatonin the hormone that helps you sleep.
Late afternoon caffeine might seem harmless, but it can stick around in your system for hours.
Overthinking tomorrow’s to-do list while lying in bed? It signals your brain that there’s still work to do—even if your body is screaming for rest.
What Lack of Sleep Does to Anxiety
Here’s the tough part: the less sleep you get, the worse your anxiety becomes the next day. That brain fog? The irritability? The restlessness? They all feed back into the same loop, making sleep even harder the following night.
It’s a cycle that wears you down mentally, emotionally, and even physically.
So What Can You Do?
Breaking the cycle doesn’t happen overnight (pun intended), but small changes go a long way:
Create a wind-down routine: Start dimming the lights an hour before bed. Stretch. Read. Journal. Do anything calming away from screens.
Cut back on stimulants: Limit caffeine after noon and avoid sugary snacks late in the day.
Try grounding techniques: Breathing exercises or body scans can calm the nervous system and shift your body into “rest mode.”
Stick to a sleep schedule: Try to sleep and wake at the same time every day even on weekends. Consistency helps reset your internal clock.
When to Talk to Someone
If your sleep struggles persist for weeks, or if your anxiety feels overwhelming, talk to a professional. Therapy or even short-term medication can help break the cycle and give you space to heal mentally and physically.
Final Thoughts
You’re not lazy. You’re not broken. Your body is simply trying to survive in a world that doesn’t always slow down. The first step to getting better sleep might just be giving yourself grace and realizing that rest is just as much mental as it is physical.
Take it one night at a timeTired But Can’t Sleep? The Hidden Link Between Anxiety and Insomnia Ever crawl into bed, physically exhausted, but your mind just won’t shut up? You toss. You turn. You check the clock. Again. And despite needing rest more than ever, your body refuses to power down. Sound familiar? You’re not alone and you’re not just “thinking too much.” This frustrating cycle of being tired but sleepless is often rooted in anxiety, and the connection runs deeper than most people realize. The Silent Tug-of-War Between Your Mind and Body When you’re anxious whether it's from everyday stress or a deeper mental health issue your brain kicks into high alert. Your heart rate might stay elevated. Your thoughts start racing. Your body stays in “fight or flight” mode, even when it’s bedtime. And no matter how tired you feel, your brain acts like it’s preparing for battle. It’s like hitting the brakes and the gas pedal at the same time. Everyday Habits That Make It Worse Without even knowing it, some of our daily routines quietly feed this cycle. For example: Endless scrolling before bed overstimulates the brain and floods your system with blue light, which blocks melatonin the hormone that helps you sleep. Late afternoon caffeine might seem harmless, but it can stick around in your system for hours. Overthinking tomorrow’s to-do list while lying in bed? It signals your brain that there’s still work to do—even if your body is screaming for rest. What Lack of Sleep Does to Anxiety Here’s the tough part: the less sleep you get, the worse your anxiety becomes the next day. That brain fog? The irritability? The restlessness? They all feed back into the same loop, making sleep even harder the following night. It’s a cycle that wears you down mentally, emotionally, and even physically. So What Can You Do? Breaking the cycle doesn’t happen overnight (pun intended), but small changes go a long way: Create a wind-down routine: Start dimming the lights an hour before bed. Stretch. Read. Journal. Do anything calming away from screens. Cut back on stimulants: Limit caffeine after noon and avoid sugary snacks late in the day. Try grounding techniques: Breathing exercises or body scans can calm the nervous system and shift your body into “rest mode.” Stick to a sleep schedule: Try to sleep and wake at the same time every day even on weekends. Consistency helps reset your internal clock. When to Talk to Someone If your sleep struggles persist for weeks, or if your anxiety feels overwhelming, talk to a professional. Therapy or even short-term medication can help break the cycle and give you space to heal mentally and physically. Final Thoughts You’re not lazy. You’re not broken. Your body is simply trying to survive in a world that doesn’t always slow down. The first step to getting better sleep might just be giving yourself grace and realizing that rest is just as much mental as it is physical. Take it one night at a time0 Comments 0 Shares 966 Views1
-
“The Pressure to Have It All Together Is Affecting Your Health — Here’s How”
Lately, have you felt constantly drained, on edge, or like you're always “on” even when your body just wants to rest? You’re not alone. Many of us live under the silent pressure to keep everything together—at work, at home, in our relationships—often at the expense of our own well-being. The truth is, this pressure doesn’t just affect your mood.
Mental Load = Physical Stress
When your brain is juggling 10 things at once—deadlines, family responsibilities, unread messages it’s in a near-constant state of alert. This mental load can lead to chronic stress, which in turn affects your sleep, digestion, immune system, and heart health. You might think you're just tired, but your body is actually reacting to emotional strain.
You're Probably Not Lazy You’re Burnt Out
If you've been waking up exhausted or struggling to concentrate, there's a chance you're not just being “lazy” or “unmotivated.” These can be signs of burnout or mental fatigue. Burnout is now recognized as a legitimate health condition by the World Health Organization—it’s your brain's way of saying “enough.”
The Hidden Toll of Suppressing Emotions
Burying your feelings to appear strong or “fine” can lead to somatic symptoms—things like tension headaches, stomach discomfort, body aches, or even high blood pressure. Emotional health is deeply tied to physical health, and ignoring one often disrupts the other.
Social Media Can Make It Worse
We see highlight reels of other people’s lives, and without realizing it, we compare. But comparison is a silent stressor. It can heighten anxiety, lower self-esteem, and fuel the pressure to appear put-together even when you’re falling apart inside.
Let’s Normalize Taking a Step Back
Your mind and body were not designed to be in overdrive all the time. Taking breaks, saying “no,” and getting support whether it’s from a friend or a therapist isn’t a luxury. It’s healthcare. Mental health is not something extra. It’s part of your total health.
Final Thought
You’re allowed to not be okay sometimes. And you don’t need to hit a crisis point to take care of yourself. Pay attention to your body’s signals. Exhaustion, mood swings, poor sleep, and frequent illnesses could all be signs that you’re doing too much. You matter—and so does your health.“The Pressure to Have It All Together Is Affecting Your Health — Here’s How” Lately, have you felt constantly drained, on edge, or like you're always “on” even when your body just wants to rest? You’re not alone. Many of us live under the silent pressure to keep everything together—at work, at home, in our relationships—often at the expense of our own well-being. The truth is, this pressure doesn’t just affect your mood. Mental Load = Physical Stress When your brain is juggling 10 things at once—deadlines, family responsibilities, unread messages it’s in a near-constant state of alert. This mental load can lead to chronic stress, which in turn affects your sleep, digestion, immune system, and heart health. You might think you're just tired, but your body is actually reacting to emotional strain. You're Probably Not Lazy You’re Burnt Out If you've been waking up exhausted or struggling to concentrate, there's a chance you're not just being “lazy” or “unmotivated.” These can be signs of burnout or mental fatigue. Burnout is now recognized as a legitimate health condition by the World Health Organization—it’s your brain's way of saying “enough.” The Hidden Toll of Suppressing Emotions Burying your feelings to appear strong or “fine” can lead to somatic symptoms—things like tension headaches, stomach discomfort, body aches, or even high blood pressure. Emotional health is deeply tied to physical health, and ignoring one often disrupts the other. Social Media Can Make It Worse We see highlight reels of other people’s lives, and without realizing it, we compare. But comparison is a silent stressor. It can heighten anxiety, lower self-esteem, and fuel the pressure to appear put-together even when you’re falling apart inside. Let’s Normalize Taking a Step Back Your mind and body were not designed to be in overdrive all the time. Taking breaks, saying “no,” and getting support whether it’s from a friend or a therapist isn’t a luxury. It’s healthcare. Mental health is not something extra. It’s part of your total health. Final Thought You’re allowed to not be okay sometimes. And you don’t need to hit a crisis point to take care of yourself. Pay attention to your body’s signals. Exhaustion, mood swings, poor sleep, and frequent illnesses could all be signs that you’re doing too much. You matter—and so does your health.0 Comments 0 Shares 979 Views -
“Bloating Isn’t Just From Food — Here’s What Your Body Might Be Telling You”
Ever feel like your tummy turns into a balloon after eating, even when you didn’t overeat?
You’re not alone. Bloating can make you feel uncomfortable, sluggish, and sometimes even embarrassed. While food does play a role, it’s not always the usual suspects like beans or carbonated drinks. Sometimes, your body is trying to tell you something deeper.
Let’s decode the real reasons behind that “why do I feel 6 months pregnant?” belly bloat:
Stress is a Sneaky Culprit
Believe it or not, your gut has a direct line to your brain. When you’re stressed, anxious, or overwhelmed, your digestive system can slow down or spasm, causing bloating. That bloated feeling after a long day might not be from lunch, it might be from life.
You’re Not Drinking Enough Water
Hydration helps your digestive system move things along. When you’re dehydrated, digestion becomes sluggish, leading to constipation and you guessed it;bloating. Aim to sip water throughout the day (not just when you're thirsty).
Your Gut Might Be Out of Balance
If you’re constantly bloated, your gut microbiome might need help. A lack of good bacteria can slow digestion and cause gas buildup. Consider adding fermented foods (like yogurt, kefir, or kimchi) to your meals—or speak to a doctor about probiotics.
Gas Traps in Fizzy Drinks and Sweeteners
Carbonated drinks literally fill your stomach with air. And artificial sweeteners like sorbitol or xylitol (found in sugar-free gum and snacks) can ferment in your gut, causing gas and discomfort. Not all "sugar-free" foods are bloat-free.
Irregular Bowel Movements = A Backed-Up System
If you’re not “going” regularly, you’re likely going to feel it. Constipation can trap gas and make you feel bloated for days. Your gut is like traffic; when there's a hold-up, everything else slows down too.
Red Flags: When to Take It Seriously
Occasional bloating is normal. But if it’s always there, especially with weight loss, fatigue, nausea, or changes in your stool, please don’t ignore it. These could be signs of something more serious like IBS, food intolerances, or even ovarian issues.
Final Thought:
Your body is constantly sending you signals. That bloated belly may be louder than usual, but it’s just trying to get your attention. Listen closely, and treat it with care.0 Comments 0 Shares 325 Views1
-
“Bloating Isn’t Just From Food — Here’s What Your Body Might Be Telling You”
Ever feel like your tummy turns into a balloon after eating, even when you didn’t overeat?
You’re not alone. Bloating can make you feel uncomfortable, sluggish, and sometimes even embarrassed. While food does play a role, it’s not always the usual suspects like beans or carbonated drinks. Sometimes, your body is trying to tell you something deeper.
Let’s decode the real reasons behind that “why do I feel 6 months pregnant?” belly bloat:
Stress is a Sneaky Culprit
Believe it or not, your gut has a direct line to your brain. When you’re stressed, anxious, or overwhelmed, your digestive system can slow down or spasm, causing bloating. That bloated feeling after a long day might not be from lunch, it might be from life.
You’re Not Drinking Enough Water
Hydration helps your digestive system move things along. When you’re dehydrated, digestion becomes sluggish, leading to constipation and you guessed it;bloating. Aim to sip water throughout the day (not just when you're thirsty).
Your Gut Might Be Out of Balance
If you’re constantly bloated, your gut microbiome might need help. A lack of good bacteria can slow digestion and cause gas buildup. Consider adding fermented foods (like yogurt, kefir, or kimchi) to your meals—or speak to a doctor about probiotics.
Gas Traps in Fizzy Drinks and Sweeteners
Carbonated drinks literally fill your stomach with air. And artificial sweeteners like sorbitol or xylitol (found in sugar-free gum and snacks) can ferment in your gut, causing gas and discomfort. Not all "sugar-free" foods are bloat-free.
Irregular Bowel Movements = A Backed-Up System
If you’re not “going” regularly, you’re likely going to feel it. Constipation can trap gas and make you feel bloated for days. Your gut is like traffic; when there's a hold-up, everything else slows down too.
Red Flags: When to Take It Seriously
Occasional bloating is normal. But if it’s always there, especially with weight loss, fatigue, nausea, or changes in your stool, please don’t ignore it. These could be signs of something more serious like IBS, food intolerances, or even ovarian issues.
Final Thought:
Your body is constantly sending you signals. That bloated belly may be louder than usual, but it’s just trying to get your attention. Listen closely, and treat it with care.🍞 “Bloating Isn’t Just From Food — Here’s What Your Body Might Be Telling You” Ever feel like your tummy turns into a balloon after eating, even when you didn’t overeat? You’re not alone. Bloating can make you feel uncomfortable, sluggish, and sometimes even embarrassed. While food does play a role, it’s not always the usual suspects like beans or carbonated drinks. Sometimes, your body is trying to tell you something deeper. Let’s decode the real reasons behind that “why do I feel 6 months pregnant?” belly bloat: 🧠 Stress is a Sneaky Culprit Believe it or not, your gut has a direct line to your brain. When you’re stressed, anxious, or overwhelmed, your digestive system can slow down or spasm, causing bloating. That bloated feeling after a long day might not be from lunch, it might be from life. 💧 You’re Not Drinking Enough Water Hydration helps your digestive system move things along. When you’re dehydrated, digestion becomes sluggish, leading to constipation and you guessed it;bloating. Aim to sip water throughout the day (not just when you're thirsty). 🐌 Your Gut Might Be Out of Balance If you’re constantly bloated, your gut microbiome might need help. A lack of good bacteria can slow digestion and cause gas buildup. Consider adding fermented foods (like yogurt, kefir, or kimchi) to your meals—or speak to a doctor about probiotics. 🥤 Gas Traps in Fizzy Drinks and Sweeteners Carbonated drinks literally fill your stomach with air. And artificial sweeteners like sorbitol or xylitol (found in sugar-free gum and snacks) can ferment in your gut, causing gas and discomfort. Not all "sugar-free" foods are bloat-free. 🚽 Irregular Bowel Movements = A Backed-Up System If you’re not “going” regularly, you’re likely going to feel it. Constipation can trap gas and make you feel bloated for days. Your gut is like traffic; when there's a hold-up, everything else slows down too. ⚠️ Red Flags: When to Take It Seriously Occasional bloating is normal. But if it’s always there, especially with weight loss, fatigue, nausea, or changes in your stool, please don’t ignore it. These could be signs of something more serious like IBS, food intolerances, or even ovarian issues. 💬 Final Thought: Your body is constantly sending you signals. That bloated belly may be louder than usual, but it’s just trying to get your attention. Listen closely, and treat it with care. 🌿✨0 Comments 1 Shares 691 Views1
-
Mental Exhaustion Is Real — And It’s Not Just ‘Laziness’
Ever felt like your brain is carrying bricks even after sleeping all night? You're not alone. That constant tiredness, lack of motivation, and urge to just do nothing could be mental exhaustion; not laziness like people often assume.
Let’s talk about it
😵💫 You Wake Up Tired Every. Single. Day.
It’s not always about the hours of sleep. If your mind is constantly in overdrive — worrying, planning, multitasking , it never really shuts down. So even after 8 hours in bed, you might still feel like you’ve run a marathon.
Digital Overload Is Draining You
From morning till night, we’re staring at screens ; work, WhatsApp, Instagram, YouTube, repeat. Your brain never gets a real break, and it’s silently screaming for one. No wonder you're feeling drained.
Too Many Tabs Open (In Your Head)
That endless to-do list? Mental exhaustion loves that. If you’re constantly juggling responsibilities without taking time to breathe, you’ll crash — mentally, emotionally, and even physically.
People Don’t See It — So They Think You’re Fine
Mental exhaustion doesn’t come with a bandage or fever. So people assume you’re just being lazy, moody, or “not serious.” But your brain might be quietly begging for rest.
So… What Can You Do?
Give your brain a break ; Schedule short, device-free quiet times. No scrolling, no calls. Just be.
Learn to say NO , You don’t have to be everything for everyone. Boundaries = peace.
Sleep, but the right kind; Create a routine. No caffeine at night. No phones in bed.
Move your body , A walk, dancing, or stretching. Movement boosts mental clarity.
Talk about it , You’re not weak. You’re human. Share how you feel with someone you trust.
Final Thought
You’re not lazy. You’re tired mentally. It’s okay to pause. It’s okay to reset.
Taking care of your mind is just as important as taking care of your body.
So the next time someone says, “Why are you always tired?”
Look them in the eye and say, “Because mental exhaustion is real.”🧠 Mental Exhaustion Is Real — And It’s Not Just ‘Laziness’ Ever felt like your brain is carrying bricks even after sleeping all night? You're not alone. That constant tiredness, lack of motivation, and urge to just do nothing could be mental exhaustion; not laziness like people often assume. Let’s talk about it 👇 😵💫 You Wake Up Tired Every. Single. Day. It’s not always about the hours of sleep. If your mind is constantly in overdrive — worrying, planning, multitasking , it never really shuts down. So even after 8 hours in bed, you might still feel like you’ve run a marathon. 📱 Digital Overload Is Draining You From morning till night, we’re staring at screens ; work, WhatsApp, Instagram, YouTube, repeat. Your brain never gets a real break, and it’s silently screaming for one. No wonder you're feeling drained. 🧾 Too Many Tabs Open (In Your Head) That endless to-do list? Mental exhaustion loves that. If you’re constantly juggling responsibilities without taking time to breathe, you’ll crash — mentally, emotionally, and even physically. 😔 People Don’t See It — So They Think You’re Fine Mental exhaustion doesn’t come with a bandage or fever. So people assume you’re just being lazy, moody, or “not serious.” But your brain might be quietly begging for rest. 🧘♀️ So… What Can You Do? 💡 Give your brain a break ; Schedule short, device-free quiet times. No scrolling, no calls. Just be. 💡 Learn to say NO , You don’t have to be everything for everyone. Boundaries = peace. 💡 Sleep, but the right kind; Create a routine. No caffeine at night. No phones in bed. 💡 Move your body , A walk, dancing, or stretching. Movement boosts mental clarity. 💡 Talk about it , You’re not weak. You’re human. Share how you feel with someone you trust. 💬 Final Thought You’re not lazy. You’re tired mentally. It’s okay to pause. It’s okay to reset. Taking care of your mind is just as important as taking care of your body. So the next time someone says, “Why are you always tired?” Look them in the eye and say, “Because mental exhaustion is real.” 💯1 Comments 0 Shares 789 Views1
-
Too Much Seasoning, Too Little Health: The Silent Danger in Your Kitchen”
Let’s talk about something sitting quietly in almost every Nigerian kitchen seasoning cubes.
You know them well. The “flavour masters.” The small but mighty cubes that transform a basic pot of soup into something your neighbours will smell three compounds away. But here’s the not-so-sweet truth: those little blocks of magic could be slowly damaging your health, one delicious bite at a time.
1. Seasoning Cubes Are Sodium Bombs in Disguise
Seasoning cubes are more than just spices. They’re loaded with salt (sodium) and MSG (monosodium glutamate). Yes, they taste amazing, but too much sodium can silently harm your heart and kidneys.
Tired all the time? Swollen feet? High blood pressure at a young age? Your seasoning habit could be one of the hidden culprits.
2. “But I Don’t Even Add Salt!” That Doesn’t Mean You’re Safe
This is where most people miss it.
You don’t need to sprinkle salt for your sodium levels to be too high. Just one or two cubes per meal might already exceed the recommended daily limit. And when you combine that with salty snacks, suya, white bread, and processed foods… your body is overloaded before you even realize it.
3. Your Kidneys Are Not Indestructible
Your kidneys work hard every day to filter your blood and manage your body’s salt balance. But constantly forcing them to process excess sodium? That’s like making them work overtime every single day with no rest. Over time, fatigue, swelling, and even kidney failure can sneak in.
And once those symptoms show up, treatment is often expensive and stressful.
4. MSG Reactions Are Real — Even if You Haven’t Noticed Yet
Some people are sensitive to MSG and don’t even realize it. It can cause headaches, sweating, tingling, a fast heartbeat, anxiety, or a general “off” feeling after eating.
So if you’ve ever finished a tasty meal and felt strangely uncomfortable afterward… it might be your body quietly protesting.
5. How to Keep Your Food Tasty and Safe
Don’t worry no one’s asking you to eat bland meals. There are plenty of ways to keep your food rich and flavourful without overloading on cubes:
Use real ingredients: onions, garlic, ginger, local herbs, curry, thyme, scent leaf, turmeric, uziza… all packed with natural flavour.
Cut down gradually: Instead of 3 cubes, try 1. Your taste buds will adjust over time.
Taste first, cube later: Most times, the food is already well-seasoned.
Educate with love: Help others around you (mama, aunty, house help) understand this. It’s not criticism, it’s care.
Final Word: Let Your Food Heal, Not Harm
You deserve to enjoy delicious meals — but not at the cost of your health.
That sweet stew, that rich jollof, that smoky native soup — let it be both enjoyable and safe.
Because life is already hard enough — your food shouldn’t be what slowly breaks you down.Too Much Seasoning, Too Little Health: The Silent Danger in Your Kitchen” Let’s talk about something sitting quietly in almost every Nigerian kitchen seasoning cubes. You know them well. The “flavour masters.” The small but mighty cubes that transform a basic pot of soup into something your neighbours will smell three compounds away. But here’s the not-so-sweet truth: those little blocks of magic could be slowly damaging your health, one delicious bite at a time. 1. Seasoning Cubes Are Sodium Bombs in Disguise Seasoning cubes are more than just spices. They’re loaded with salt (sodium) and MSG (monosodium glutamate). Yes, they taste amazing, but too much sodium can silently harm your heart and kidneys. Tired all the time? Swollen feet? High blood pressure at a young age? Your seasoning habit could be one of the hidden culprits. 2. “But I Don’t Even Add Salt!” That Doesn’t Mean You’re Safe This is where most people miss it. You don’t need to sprinkle salt for your sodium levels to be too high. Just one or two cubes per meal might already exceed the recommended daily limit. And when you combine that with salty snacks, suya, white bread, and processed foods… your body is overloaded before you even realize it. 3. Your Kidneys Are Not Indestructible Your kidneys work hard every day to filter your blood and manage your body’s salt balance. But constantly forcing them to process excess sodium? That’s like making them work overtime every single day with no rest. Over time, fatigue, swelling, and even kidney failure can sneak in. And once those symptoms show up, treatment is often expensive and stressful. 4. MSG Reactions Are Real — Even if You Haven’t Noticed Yet Some people are sensitive to MSG and don’t even realize it. It can cause headaches, sweating, tingling, a fast heartbeat, anxiety, or a general “off” feeling after eating. So if you’ve ever finished a tasty meal and felt strangely uncomfortable afterward… it might be your body quietly protesting. 5. How to Keep Your Food Tasty and Safe Don’t worry no one’s asking you to eat bland meals. There are plenty of ways to keep your food rich and flavourful without overloading on cubes: ✅ Use real ingredients: onions, garlic, ginger, local herbs, curry, thyme, scent leaf, turmeric, uziza… all packed with natural flavour. ✅ Cut down gradually: Instead of 3 cubes, try 1. Your taste buds will adjust over time. ✅ Taste first, cube later: Most times, the food is already well-seasoned. ✅ Educate with love: Help others around you (mama, aunty, house help) understand this. It’s not criticism, it’s care. 🍲 Final Word: Let Your Food Heal, Not Harm You deserve to enjoy delicious meals — but not at the cost of your health. That sweet stew, that rich jollof, that smoky native soup — let it be both enjoyable and safe. Because life is already hard enough — your food shouldn’t be what slowly breaks you down.0 Comments 0 Shares 902 Views1
-
“When Mouth Problems Speak Louder Than Words: What Your Oral Health Says About You”
Introduction:
When was the last time you paid attention to your mouth—not just for a selfie, but really paid attention? Many people treat oral hygiene like a separate department in the health store, but your mouth might be trying to tell you what’s going on in your body. Bleeding gums, dry mouth, bad breath, and loose teeth might be more than dental issues—they could be early warning signs of something bigger.
1. Gum Disease and Your Heart—A Hidden Link
Studies show a strong connection between periodontal (gum) disease and heart disease. The bacteria that cause inflamed gums can enter your bloodstream and trigger inflammation in your arteries, increasing your risk for heart attack and stroke. If your gums bleed often when you brush, it’s worth more than just switching toothbrushes—it could mean your heart is at risk too.
2. Bad Breath Isn’t Always About What You Ate
Garlic and onions aside, persistent bad breath (halitosis) can be a sign of underlying health issues. It could indicate diabetes (especially if it smells fruity), acid reflux, liver disease, or even kidney problems. Don’t just reach for mints—find the root cause.
3. Oral Health and Brain Function—More Connected Than You Think
Did you know that oral bacteria have been found in the brains of people with Alzheimer’s? While research is ongoing, poor oral hygiene may contribute to cognitive decline. The inflammation that starts in the mouth can travel and possibly affect brain function.
4. Loose Teeth and Bone Health
If your teeth suddenly start shifting or loosening, it could indicate bone loss—not just in your jaw, but possibly throughout your body. This might point to osteoporosis or nutritional deficiencies, especially in women.
5. Habits That Hurt Without You Knowing
Chewing ice: It might feel satisfying but it weakens enamel.
Over-brushing: Hard bristles or aggressive brushing can erode gum lines.
Skipping flossing: Brushing alone only cleans 60% of your teeth.
Constant snacking: Sugar isn’t the only culprit—frequent snacking feeds bacteria all day.
Conclusion: Your Mouth Is a Messenger
Your oral health is a silent communicator of your body’s internal state. Don’t ignore the signs. Regular dental visits, proper hygiene, and paying attention to changes in your mouth can help prevent not only tooth decay but potentially serious systemic diseases.
Remember: Healthy mouth, healthy body.🦷 “When Mouth Problems Speak Louder Than Words: What Your Oral Health Says About You” Introduction: When was the last time you paid attention to your mouth—not just for a selfie, but really paid attention? Many people treat oral hygiene like a separate department in the health store, but your mouth might be trying to tell you what’s going on in your body. Bleeding gums, dry mouth, bad breath, and loose teeth might be more than dental issues—they could be early warning signs of something bigger. 1. Gum Disease and Your Heart—A Hidden Link Studies show a strong connection between periodontal (gum) disease and heart disease. The bacteria that cause inflamed gums can enter your bloodstream and trigger inflammation in your arteries, increasing your risk for heart attack and stroke. If your gums bleed often when you brush, it’s worth more than just switching toothbrushes—it could mean your heart is at risk too. 2. Bad Breath Isn’t Always About What You Ate Garlic and onions aside, persistent bad breath (halitosis) can be a sign of underlying health issues. It could indicate diabetes (especially if it smells fruity), acid reflux, liver disease, or even kidney problems. Don’t just reach for mints—find the root cause. 3. Oral Health and Brain Function—More Connected Than You Think Did you know that oral bacteria have been found in the brains of people with Alzheimer’s? While research is ongoing, poor oral hygiene may contribute to cognitive decline. The inflammation that starts in the mouth can travel and possibly affect brain function. 4. Loose Teeth and Bone Health If your teeth suddenly start shifting or loosening, it could indicate bone loss—not just in your jaw, but possibly throughout your body. This might point to osteoporosis or nutritional deficiencies, especially in women. 5. Habits That Hurt Without You Knowing Chewing ice: It might feel satisfying but it weakens enamel. Over-brushing: Hard bristles or aggressive brushing can erode gum lines. Skipping flossing: Brushing alone only cleans 60% of your teeth. Constant snacking: Sugar isn’t the only culprit—frequent snacking feeds bacteria all day. Conclusion: Your Mouth Is a Messenger Your oral health is a silent communicator of your body’s internal state. Don’t ignore the signs. Regular dental visits, proper hygiene, and paying attention to changes in your mouth can help prevent not only tooth decay but potentially serious systemic diseases. Remember: Healthy mouth, healthy body. 🪥❤️0 Comments 0 Shares 696 Views -
Is Your Phone Making You Sick? The Hidden Health Hazards of Constant Screen Time
In today's fast-paced, digital-first world, our phones have become almost an extension of ourselves. From morning alarms to late-night scrolling, smartphones are constantly in our hands. But while these devices keep us connected, informed, and entertained, could they also be silently sabotaging our health?
1. Eye Strain and Vision Problems
Prolonged screen time leads to digital eye strain, also known as computer vision syndrome. Symptoms include dry eyes, blurred vision, and headaches. Blue light from screens can also disrupt sleep patterns by affecting melatonin production.
2. Poor Posture and "Tech Neck"
Leaning over your phone for hours strains the neck and back, contributing to poor posture and chronic pain. This phenomenon, often called "tech neck," can lead to long-term spinal issues if not addressed early.
3. Mental Health Concerns
Overuse of social media and constant connectivity have been linked to increased anxiety, depression, and feelings of inadequacy. The pressure to stay updated or compare oneself to curated online lives can take a toll on mental well-being.
4. Sleep Disruption
Using your phone right before bed can interfere with your sleep quality. Blue light suppresses melatonin, the hormone that regulates sleep, making it harder to fall and stay asleep.
5. Germs on Your Screen
Your phone may be dirtier than a public toilet seat. We take our phones everywhere, including the bathroom, and rarely clean them. Constant touching spreads bacteria, increasing your risk of illness.
How to Protect Your Health:
Follow the 20-20-20 rule: Every 20 minutes, look at something 20 feet away for 20 seconds.
Limit screen time, especially at night. Consider using night mode or blue light filters.
Maintain good posture and take breaks to stretch.
Clean your phone regularly with a disinfectant wipe.
Schedule "digital detox" periods to disconnect and recharge.
Conclusion:
Your smartphone is a powerful tool, but like all tools, it needs to be used wisely. By being aware of its potential health impacts and adopting healthy screen habits, you can stay connected without compromising your well-being.
Is Your Phone Making You Sick? The Hidden Health Hazards of Constant Screen Time In today's fast-paced, digital-first world, our phones have become almost an extension of ourselves. From morning alarms to late-night scrolling, smartphones are constantly in our hands. But while these devices keep us connected, informed, and entertained, could they also be silently sabotaging our health? 1. Eye Strain and Vision Problems Prolonged screen time leads to digital eye strain, also known as computer vision syndrome. Symptoms include dry eyes, blurred vision, and headaches. Blue light from screens can also disrupt sleep patterns by affecting melatonin production. 2. Poor Posture and "Tech Neck" Leaning over your phone for hours strains the neck and back, contributing to poor posture and chronic pain. This phenomenon, often called "tech neck," can lead to long-term spinal issues if not addressed early. 3. Mental Health Concerns Overuse of social media and constant connectivity have been linked to increased anxiety, depression, and feelings of inadequacy. The pressure to stay updated or compare oneself to curated online lives can take a toll on mental well-being. 4. Sleep Disruption Using your phone right before bed can interfere with your sleep quality. Blue light suppresses melatonin, the hormone that regulates sleep, making it harder to fall and stay asleep. 5. Germs on Your Screen Your phone may be dirtier than a public toilet seat. We take our phones everywhere, including the bathroom, and rarely clean them. Constant touching spreads bacteria, increasing your risk of illness. How to Protect Your Health: Follow the 20-20-20 rule: Every 20 minutes, look at something 20 feet away for 20 seconds. Limit screen time, especially at night. Consider using night mode or blue light filters. Maintain good posture and take breaks to stretch. Clean your phone regularly with a disinfectant wipe. Schedule "digital detox" periods to disconnect and recharge. Conclusion: Your smartphone is a powerful tool, but like all tools, it needs to be used wisely. By being aware of its potential health impacts and adopting healthy screen habits, you can stay connected without compromising your well-being.0 Comments 0 Shares 638 Views
More Stories